The Tshwane initiative could help reduce drug use, drug-related crime and new HIV infections.
Tshwane residents who use opioid drugs such as heroin or whoonga can now swap their dangerous drugs of choice for something safer as part of an innovative new programme that is the first of its kind in Gauteng.
Tshwane and the University of Pretoria have begun providing opioid substitution therapy (OST) in seven clinics in central Pretoria and Tshwane townships. As part of the programme, patients undergo a means test to determine whether they qualify for free services or if they must pay between R600 and R1 500 for monthly treatment, says Jannie Hugo, University of Pretoria’s head of family medicine department.
Opioids are a class of drugs that includes not only forms of heroin but also prescription painkillers. People who regularly take opioids experience withdrawal symptoms such as nausea and muscle cramps even within hours of their last dose. The only way to avoid these symptoms is to take more of the drug.
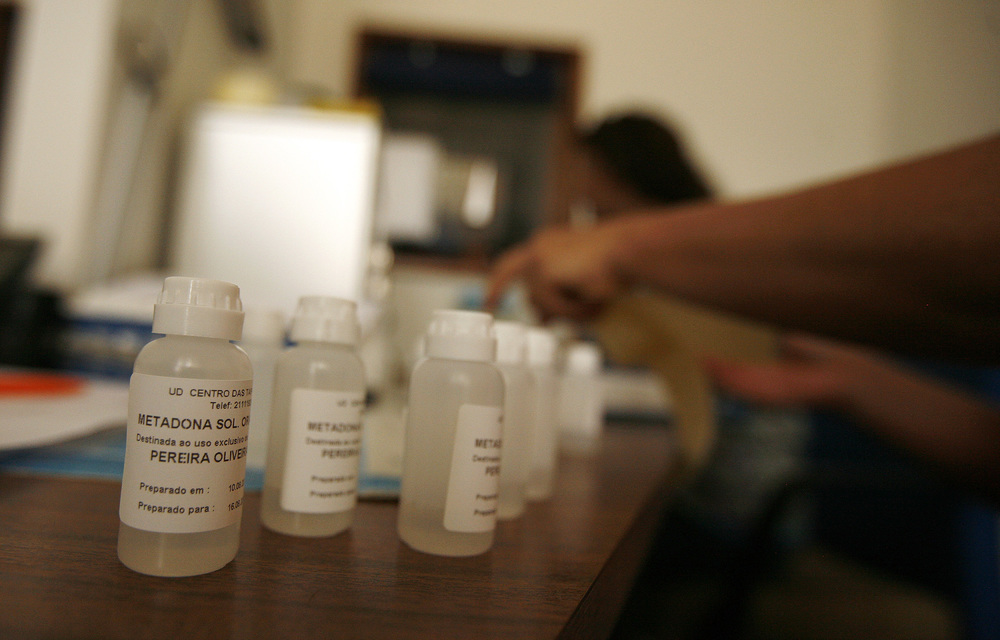
But as part of OST, doctors prescribe people who use opioids legal replacement therapies such as the drug methadone or buprenorphine that are often taken under the direct supervision of health workers or pharmacists in the case of Tshwane patients.
Although these therapies do not give people a “high”, they allow opioid users to avoid debilitating withdrawal symptoms. OST programmes have been shown to help reduce illegal drug use, criminal activity linked to drugs as well as overdose deaths and new HIV infections among people who use drugs, according to a 2011 study published in the Bulletin of the World Health Organization.
Tshwane’s OST programme also links patients to counselling and job skills as well as testing for HIV and Hepatitis C.
People who inject drugs are at a high risk of HIV and Hepatitis C infection, in part because users may share needles. A five–city study conducted in South Africa found that the HIV prevalence rate among injecting drug users was about 40% higher than that of the general population, according to 2016 research published in the International Journal of Drug Policy.
Large–scale research on the prevalence of Hepatitis C among South African drug users has yet to be published, but a small 2013 survey conducted by Pretoria’s Step Up Project found that more surveyed drug users were living with Hepatitis C than with HIV.
Tshwane’s new R17–million programme is the second OST initiative in South Africa following in the footsteps of the 2013 launched programme at Cape Town’s Sultan Bahu Treatment Centre in Mitchells Plain.
Hugo says the Gauteng programme is already seeing results in its initial two months. He says it strengthens the argument that OST should be increasingly available in the public sector – a call supported by the country’s latest HIV plan.
Hugo explains:”Our experience is that it makes a significant difference. The person is able to build a normal life as the cravings are controlled. We are of opinion that OST should be made available widely for use in primary health care as part of a comprehensive care programme to deal with substance use.”
Nelisiwe Msomi was a health reporter at Bhekisisa.