- At the end of May, South Africa moved to an increased lockdown alert level in anticipation of the country’s third wave and a rise in SARS-CoV-2 infections.
- Currently, South Africa’s epidemic is dominated and shaped by the Beta variant which was first identified in the Eastern Cape in October.
- Two other variants — Alpha and Delta — have been detected in South Africa and could potentially shape what future outbreaks look like.
South Africa officially entered its third wave on Thursday, 10 June (according to the formula the country uses) amidst a slower than expected vaccine roll-out, hampered by the lack of availability of shots.
Our infections are rising at a concerning pace.
On Thursday, when South Africa saw 9 149 new COVID cases, the proportion of tests which came out positive was 15.7% — significantly above the World Health Organisation’s (WHO) threshold of 5%, which indicates that the pandemic is out of control. The rolling seven-day average on 8 June, which is a way to look at such figures over a period of time, was 13.9%.
We don’t yet know how long or how severe this wave will be, but we do know that the country’s second wave, which started towards the end of November, caught many off-guard by hitting much earlier than anticipated — it was also a much more severe wave than anticipated.
During the first wave, the peak of daily infections was 13 944 on 24 July last year, whereas the highest number of cases during the second wave was 21 980 on 8 January 2021.
The driving force behind this sharp increase in cases was the emergence of a new form of the virus called 501Y.V2 — or as it has recently been dubbed by the World Health Organisation, the Beta variant.
What was previously thought to be a relatively stable virus had rapidly evolved in a way that helped make it more transmissible and better able to circumvent the body’s protective response against the original form of the virus.
As we approach the third wave, here’s a look at which variants are currently circulating in South Africa — and how they could potentially influence our third wave.
What variants are currently circulating in South Africa?
The main form of the SARS-CoV-2 virus in South Africa is the 501Y.V2 or Beta variant — it still accounts for over 90% of COVID cases (based on our genomic data), says Richard Lessells, who was part of the team that first identified the variant.
Lessells works at the KwaZulu-Natal Research Innovation and Sequencing Platform (KRISP) at the University of KwaZulu-Natal. KRISP is part of the Network for Genomic Surveillance in South Africa, a consortium that tracks how the coronavirus is evolving in South Africa. The consortium also monitors the virus for new mutations that may be cause for concern. They do this with something called genomic sequencing, a process which unravels the genetic code of the virus.
Since about March last year, the team has sequenced around 8 100 virus samples of SARS-CoV-2 in South Africa, Lessells says. This works out to an average of between 500 and 600 samples per month — although this number increases during waves.
By continuously tracking the virus in this way, the consortium is able to detect when new variants appear in the country.
For example, on 8 May the National Institute for Communicable Diseases (NICD) issued a statement saying South Africa had its first cases caused by the B.1.617.2 or Delta variant (first identified in India). At the time, there were five reported cases. By the end of the month, there were around 22 cases (most in people who had travelled), says Lessells.
The other variant noted by the NICD was the B.1.1.7 or Alpha variant (first identified in the United Kingdom), which, at the time, accounted for 11 local cases. Lessells says this has since increased to 43 genomically confirmed cases, which now includes cases of local transmission in people who had no history of travel to countries where the variant was circulating.
Variants 101: Explaining the different forms of the virus
Variants are versions of the SARS-CoV-2 virus that have undergone changes, or mutations, in their structure. This is something that happens to all viruses over time and most of the changes are insignificant. But in some cases, these small alterations to the genetic code of the virus can affect how it behaves, such as helping it spread more easily or causing more severe disease.
The WHO has come up with two categories of variants that pose a greater public health risk: variants of interest and variants of concern.
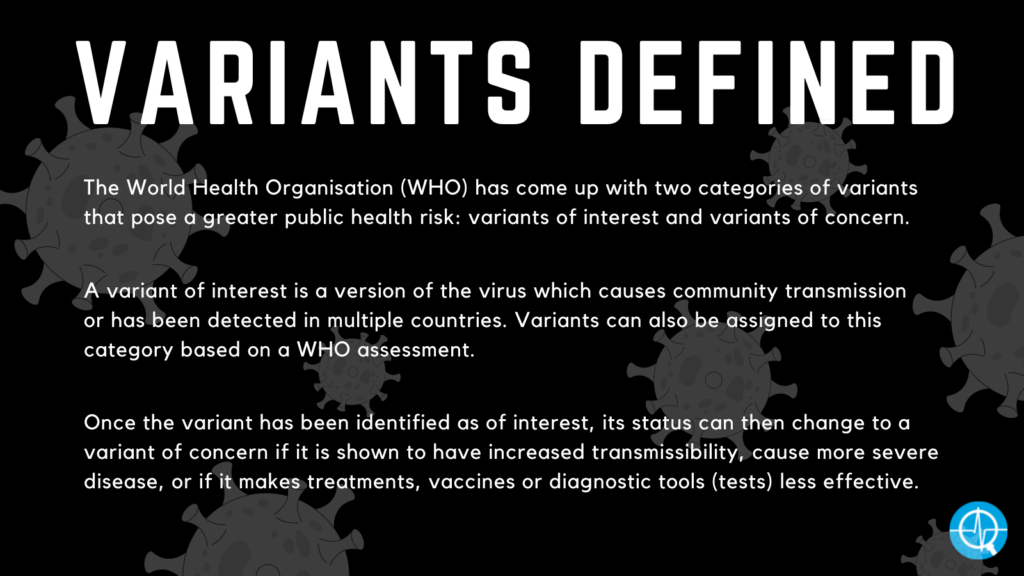
A variant of interest is a version of the virus which causes community transmission or has been detected in multiple countries. Variants can also be assigned to this category based on a WHO assessment.
Once the variant has been identified as of interest, its status can then change to a variant of concern if it is shown to have increased transmissibility, cause more severe disease, or if it makes treatments, vaccines or diagnostic tools (tests) less effective.
All three variants below are variants of concern.
• The Beta variant
Scientific names: B.1.351 or 501Y.V2
First identified: South Africa
Detected in: 115 countries
Date designated as a variant of concern: 18 December 2020
Earliest samples: August 2020
Special skills: Ability to spread more efficiently from person to person and to evade some of the body’s natural defences from previous infection or vaccination
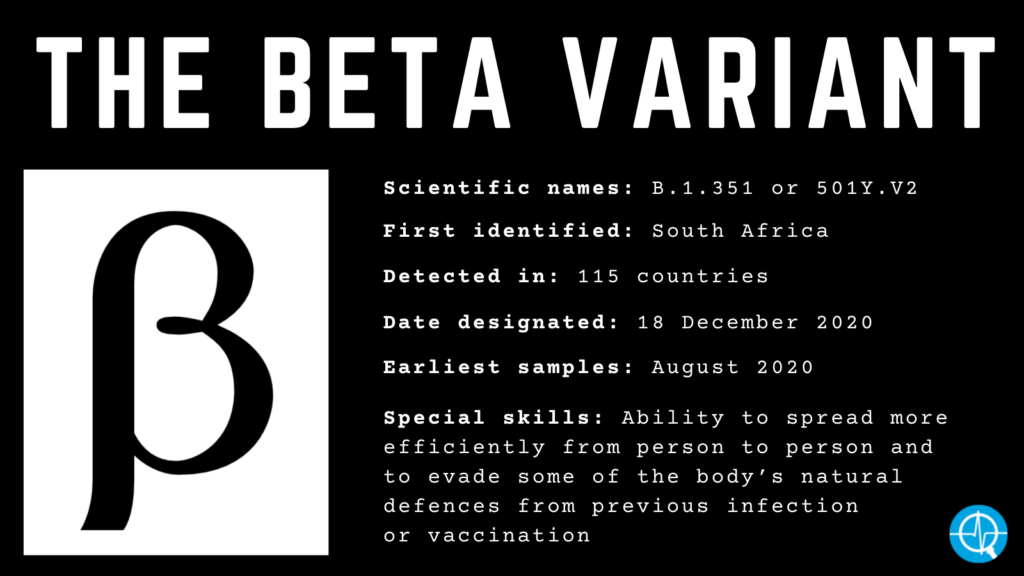
Initial studies showed the Beta variant was first detected in October last year in samples from the Eastern Cape, but Lessells says it has subsequently been detected in samples as far back as August.
The variant has over 20 changes in its structure (compared to the original form of the SARS-CoV-2 virus). On its own this is not cause for concern, but what raised alarm bells was the location of some of these mutations and their implications for the virus’s structure and function.
The spike protein sits on the surface of the virus and helps it enter your body’s cells in order to replicate. Changes to this area, as seen in the Beta variant, allow the coronavirus to better attach itself to human cells.
The Centre for the Mathematical Modelling of Infectious Diseases at the London School of Hygiene & Tropical Medicine estimates that the Beta variant is around 50% more transmissible than its original form, according to a January preprint study.
In addition to causing more infections, there is some data showing that the Beta variant is associated with more severe disease in people who were hospitalised. A May preprint study found that although the overall death toll during the second wave was not higher, the number of deaths among patients in the intensive care units increased. This increased severity in hospitalised patients was also reported in a March preprint.
Another byproduct of the changes to the virus is that it is better able to outsmart your body’s defences. One of our immune system’s first lines of attack against infections is antibodies. But mutations in the Beta variant help the virus to evade antibodies that previously helped our bodies to fight off the bug.
• The Alpha variant
Scientific names: B.1.1.7 or 501Y.V1
First identified: United Kingdom
Detected in: 161 countries
Date designated as variant of concern: 18 December 2020
Earliest samples: September 2020
Special skills: Ability to spread more efficiently from person to person
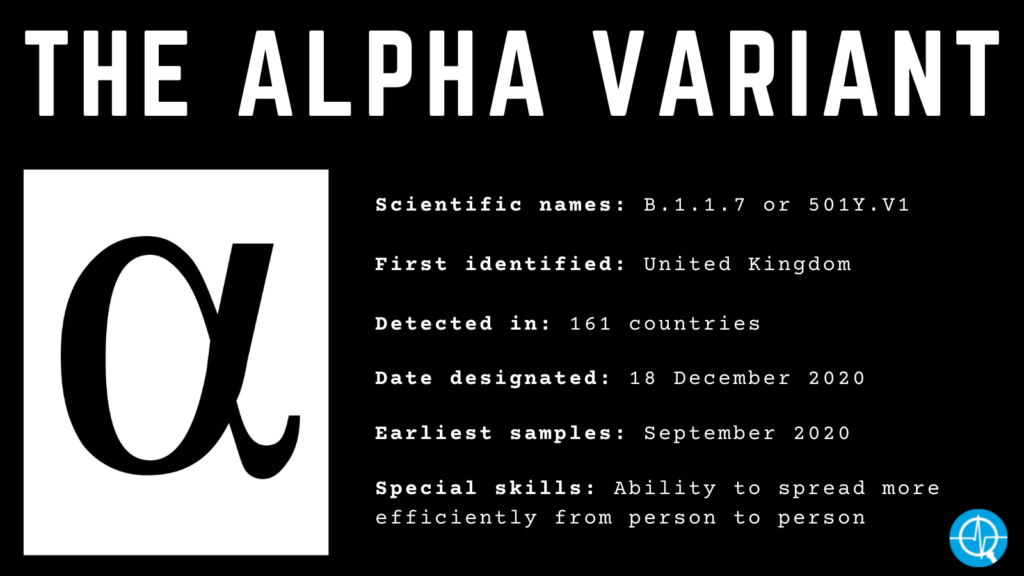
On 14 December, the United Kingdom reported that over 1 000 COVID cases caused by the Alpha variant had been identified in south-east England. Although the two variants emerged separately, there are commonalities in the structural changes between Alpha and Beta — particularly in the spike protein.
This version of the virus has 17 mutations — eight of which are located in the spike protein, where the virus attaches itself to human cells. Because these changes allow the Alpha variant to spread faster from person to person, it is estimated that it has an increased transmissibility of between 43 to 90%.
A March study published in the British Medical Journal found that the death toll from COVID cases caused by the Alpha variant had increased from 2.5 to 4.1 deaths per 1 000 detected cases. This increased mortality rate was also reported in a paper in Nature which estimated that the risk of death in cases caused by the Alpha variant was 61% higher than those caused by previous forms of the virus.
People are not at an increased risk of being reinfected with the Alpha variant. Interestingly, one of the genes deleted in this round of mutations helps make the variant easier to identify in COVID testing as the area previously targeted in the test is no longer present on the variant.
• The Delta variant
Scientific names: B.1.617.2
First identified: India
Detected in: 74 countries
Date designated as a variant of concern: 11 May 2021
Earliest samples: October 2020
Special skills: Ability to spread faster from person to person and evade immunity
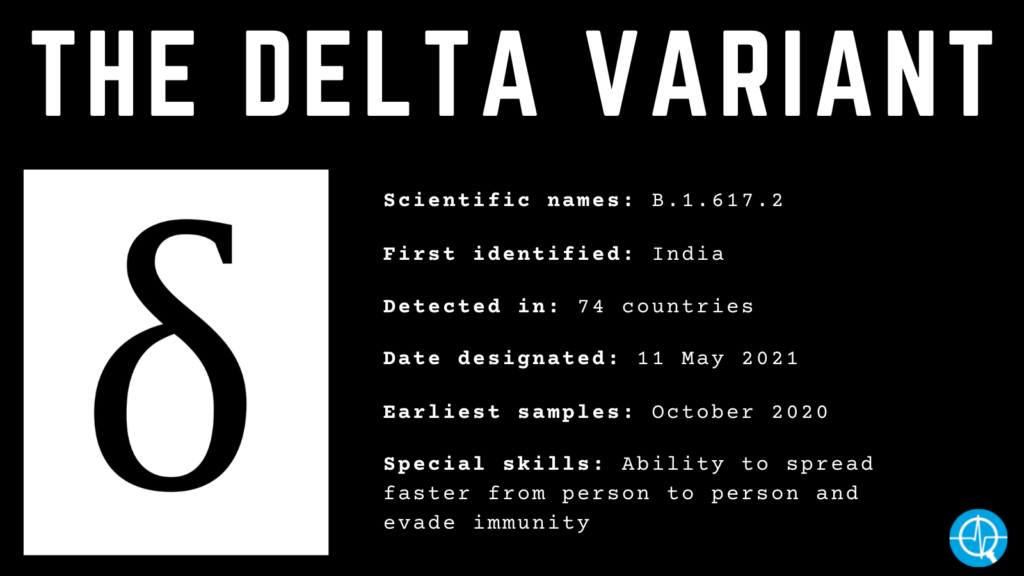
One of the newest to emerge on the list, scientists are still trying to understand the intricacies of the Delta variant. But here’s what we know so far:
The Delta variant appears to be spreading faster than the original form of SARS-CoV-2, although the exact extent to which it is doing so is unclear. Data from the United Kingdom shows that this variant is more transmissible than its local counterpart (the Alpha variant), with Delta having a secondary attack rate (an estimate of how transmissible the virus is) of 12.4% compared to Alpha’s secondary attack rate of 8.2%.
A May preprint study describes the mutations in the Delta variant’s spike protein, some of which have also been observed in other variants. These changes help the virus to better attach to your cells resulting in it spreading faster from person to person. Two of the mutations make it easier for the variant to escape immunity, rendering the antibodies our bodies produce against the original form of the virus less able to protect us against the Delta variant.
The UK data from June also shows a slight risk for increased hospitalisation when compared to the Alpha variant.
What does this mean for vaccines?
Variants which are able to evade immunity could potentially make vaccines work less well.
In the case of the Beta variant, that has turned out to be true — and there is some evidence that it may also hold true for the Delta variant.
South Africa has already seen what happens when vaccines are put to the test against the Beta variant. Both the Johnson & Johnson and AstraZeneca vaccine trials took place last year as the Beta first began circulating. Results from these trials showed how the jabs offered less protection in a South African context compared to other countries.
But this is where the baseline of a vaccine’s protection becomes important.
Just because variants can reduce a jab’s efficacy doesn’t render it completely pointless. If the starting point for protection is high enough, then even with the dip in efficacy it is still worth using.
Lessells says the effect of variants is more pronounced for mild to moderate disease, and is less so for severe disease, hospitalisation and death. “This is because protection against severe disease and death involves other arms of the immune system that are less affected by the mutations in these variants.”
So in the case of the AstraZeneca vaccine, it had an efficacy of 62% (against the original form of SARS-CoV-2) after receiving two doses. But results from the trial in South Africa found the jab’s efficacy was 21.9% in South Africa (for protection against mild to moderate COVID-19) — and this further dropped to 10.4% efficacy against cases caused by the Beta variant.
That means the Beta variant was able to reduce the vaccine’s efficacy against mild to moderate COVID-19 to the point where it was considered an inappropriate option for wide-scale roll-out in the country. (There is no data to show how well the jab protects against severe COVID caused by the Beta variant).
“That’s what this variant was able to do with the ChAdOx1 [AstraZeneca’s COVID vaccine] — it just hit it so hard that it stopped being effective and that’s what you don’t want,” says Alex Sigal, a faculty member at the Africa Health Research Institute.
As Sigal explains, vaccine efficacy is more of a hill than a straight line, so variants don’t change the efficacy of all vaccines in the same way. Instead, you have to see how the efficacy for each vaccine shifts. In the case of the AstraZeneca jab, the shift was too far and “pushed it over the edge of the cliff”, according to Sigal, which is why its efficacy dropped so dramatically.
Sigal explains: “In the end, the solution to this infection is vaccines. But if the vaccines don’t work, you’ve got a problem.”
On the other hand, Pfizer’s vaccine — which is used in South Africa’s vaccine roll-out — seems to have a stronger neutralising antibody response and is able to withstand the blow dealt by the Beta variant better. Neutralising antibodies are part of your immune system’s defence. They attach themselves to the virus in a way that stops it from infecting your cells.
The pharmaceutical company has reported that its jab had 100% efficacy against disease caused by the Beta variant and data from Qatar’s roll-out found that the jab had an effectiveness of 75% against COVID cases caused by the variant.
Although it is still too early to know if the same pattern will be seen with the Delta variant, there is some evidence suggesting that the variant does reduce vaccine efficacy. Data from cases in England showed that the effectiveness of both the Pfizer and AstraZeneca vaccines had been lowered after one dose from 51.1% to 33.5%.
But after a second shot, the decline in efficacy was smaller. In those who received the AstraZeneca jab, the efficacy had gone down from 66.1% to 59.8% and those who got the Pfizer vaccine saw a drop from 93.4% to 87.9%.
Since not all jabs are the best choice for all countries, it is important that vaccines are selected based on which jab can offer the most protection against the dominant variants circulating in a country.
“You don’t want to be playing catch up,” says Sigal. “You’d rather be in a situation where you’re protected from the get go and that’s antibodies and that means a good vaccine. That’s why these variants are kind of a pain because they can get away from at least some of these vaccines. So that’s what we need to study, especially if new variants come up that are worse than the ones we’ve got.”
Aisha Abdool Karim was a senior health reporter at Bhekisisa from 2020 to 2022.




