- In 2021, the World Health Organisation chose the South African pharmaceutical company, Afrigen Biologics, to host its mRNA vaccine technology transfer hub.
- Afrigen will invent jabs made with mRNA technology and then train manufacturers in poorer countries to make the shots as well. The first vaccine, a COVID jab, has been made and will soon be tested in clinical trials.
- We walked through Afrigen’s corridors to find out how the hub works.
Ever walked through an mRNA vaccine technology hub?
In July 2021, the World Health Organisation (WHO) and Medicines Patent Pool (MPP) launched such a centre in South Africa to make it easier for poorer countries to make their own vaccines.
In Africa, 99% of all shots given to people are imported. During the COVID-19 pandemic that meant African countries were last in line to receive jabs because manufacturers first served richer regions where the jabs were made — and who could pay more.
To help reverse this situation, the mRNA hub in South Africa will figure out how to develop new shots for diseases rampant in lower and middle-income countries and share their recipes and methods with selected manufacturers in poorer states (something international pharmaceutical companies mostly refuse to do).
In Africa’s case, this will help organisations such as the African Union and Africa Centres for Disease Control to work towards their goal to by 2040 — in less than 18 years — have the continent produce 60% of the vaccines it administers.
The hub, which is based in Cape Town, is located at the biotechnology company Afrigen Biologics, but the South African Medical Research Council also helps with research and the vaccine manufacturer, Biovac, will do larger scale production for clinical trials.
mRNA, short for messenger RNA, is the genetic code that tells a cell in your body how to make proteins. An mRNA vaccine contains the code for a specific protein that looks like it comes from the germ that causes a disease you’re trying to fight. So when you get the shot, your body makes these proteins, which, in turn, prompts your immune system to produce antibodies that will fend off the actual germ if you get infected with it.
Although mRNA technology was discovered in the 1960s, and has been tested out in other vaccines such as for flu and later also Ebola, it was only during COVID that it was used in jabs rolled out around the world.
[WATCH] Tech talk: Unpacking and assembling the puzzle pieces of a COVID vaccine
Two such jabs, one made by the pharmaceutical manufacturers Pfizer and BioNTech (we use this one in South Africa) and another by Moderna, proved to work very well.
So far, Afrigen has developed a small batch of a new mRNA COVID shot, largely based on information about Moderna’s jab and clinical trials to test how well the vaccine works will start early next year.
Because the genetic code for antigens can easily be changed using mRNA technology, this method for making vaccines can be adapted easier than more traditional methods used to make jabs. This means that Afrigen can use the same basic process for making their COVID jab to also develop vaccines for other diseases, such as HIV, tuberculosis, malaria and influenza.
In fact, Afrigen says it’s already working on finding a new, better TB jab than the one we currently give to babies.
We peered into the labs at Afrigen Biologics to find out what goes into Africa making its own shots.
The small building with the big people
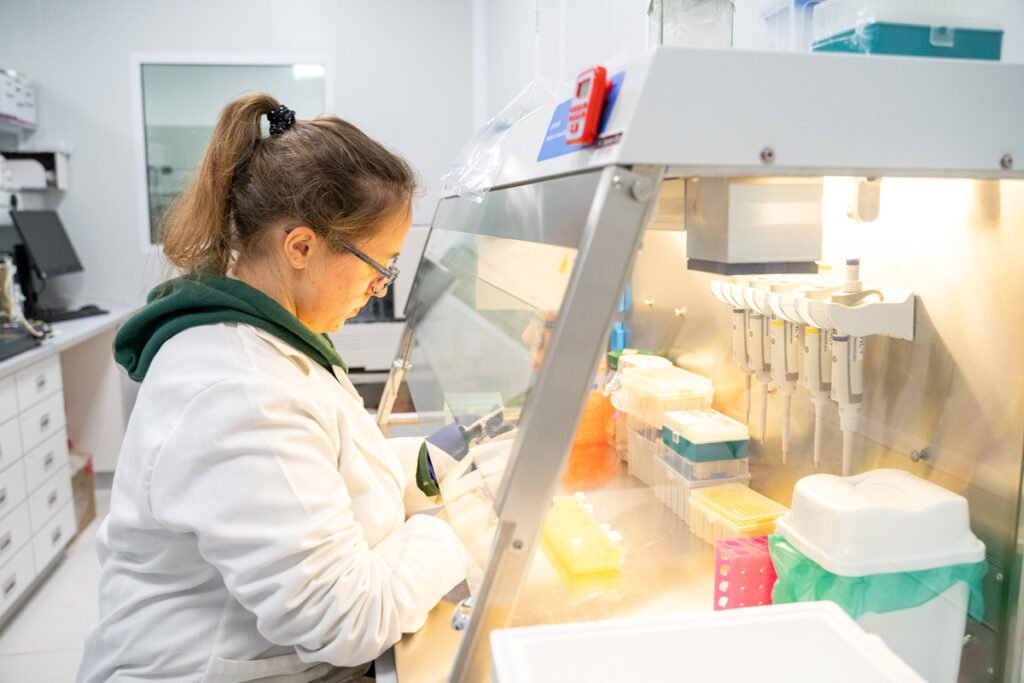
Behind a glass panel, at a workstation inside a lab, a woman scientist extracts liquid from a tray of test tubes with a piece of equipment that looks like a large syringe.
She’s testing how much genetic material there is in each test tube’s sample. This will tell her how well one of the steps in the process for making an mRNA COVID vaccine that scientists of the facility developed, is working.
The jab hasn’t yet been tested on people, but lab and animal tests look promising.
From the outside, it’s hard to tell that there are sophisticated labs in the building where the scientist is working. The two-storey red-brick building is tucked away between a plastic pipe manufacturer and a hydraulics company in the industrial area Montague Gardens, about 16 km outside of Cape Town.
But it’s here that the world’s first mRNA vaccine technology transfer hub has found a home.
Above the glass door entrance, on the side of a corrugated iron roof, an unassuming sign says Afrigen Biologics.
The scientist is working in the research and development (R&D) lab of the hub. To her right, there’s a polystyrene cooler box with more test tubes — on ice. And about a metre from her work station there’s a special machine, called a spectrophotometer, that she drips a drop of the contents from each test tube onto, to measure the amount of DNA in each tube.
“The promise of mRNA technology is phenomenal,” explains Petro Terblanche, Afrigen’s managing director. “Once you’ve established the [mRNA] platform, and therefore have a plug-and-play system, the target is that you can start manufacturing a vaccine in 90 days.”
With an mRNA platform a vaccine developer can potentially make shots for different diseases or for a new variant of a disease-causing germ without having to figure out the process from scratch each time. All that changes when you switch to working on a new shot is the genetic code with which the process starts and the quality checks during the process.
Think of it as using a ratchet wrench and socket set. The steps for making the product is the wrench; the code for making the protein that will elicit an immune response is a socket. Just like you would choose from a set of different-sized sockets to find the right fit for loosening a nut and then attaching it to the ratchet, so you could choose from mRNA sequences for different proteins and plug them into the production process one at a time.

The vaccine that the scientist is performing tests on uses the recipe of Moderna’s COVID jab as a starting point.
But because Moderna refused to share its exact methods and knowledge with Afrigen (or anyone else), Afrigen had to figure out the process themselves from documents that were available in the public domain. The end product, which Afrigen developed between September and February, is a new jab, so not an exact copy of Moderna’s shot; rather, it’s a jab that is based on the DNA code of Moderna’s vaccine.
Afrigen’s early studies in mice show that the jab not only gets the rodents’ immune systems to make antibodies, but also that the antibodies are good at inactivating the SARS-CoV-2 virus, which causes COVID. Terblanche says these results suggest that the mRNA technology they developed works.
Says Terblanche: “What COVID did is to unite the world in the quest for survival and we realised that access requires manufacturing capacity.”
Plug and play: How to start an mRNA vaccine
Across the corridor from Afrigen’s R&D lab is another, bigger one called the good manufacturing practice suite. Here scientists are covered from top to toe in white, disposable jumpsuits. The outfits protect researchers from coming into contact with bacteria or introducing potential contaminants into the process.
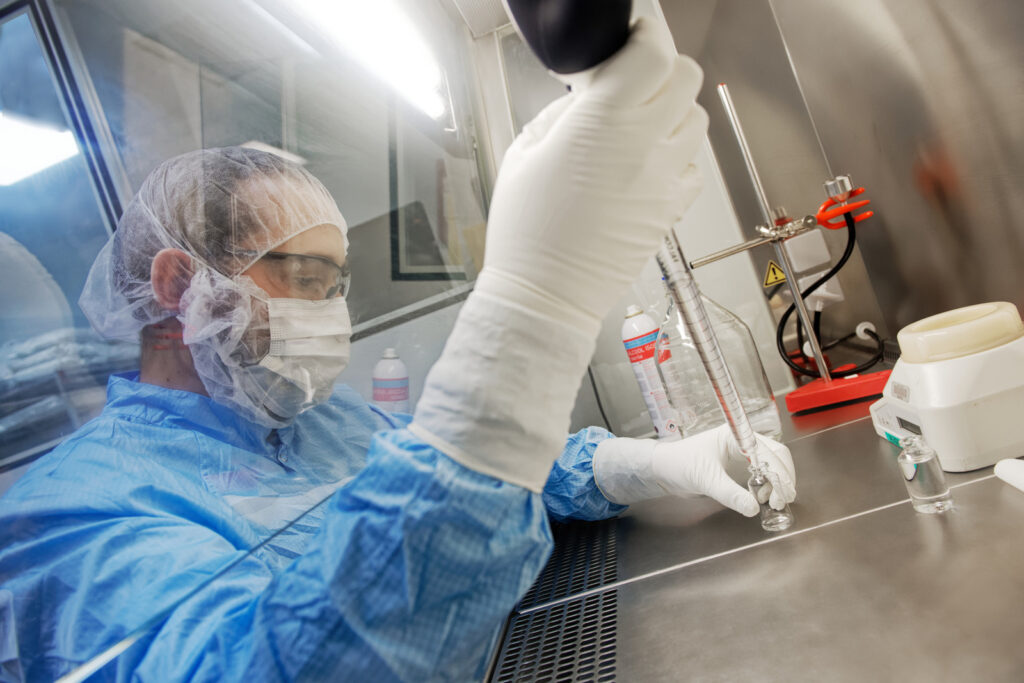
The staff is also wearing gloves and masks and there are stainless steel tanks called bioreactors, lots of tubes and pressure meters in the room.
The R&D lab is where scientists play and have fun; the manufacturing lab is where actual jabs get made.
The bioreactors are tanks in which bacteria are grown. Scientists put a ring of DNA, called a plasmid, into a small sample of bacteria to make a starter culture, almost like you would do when making a batch of yoghurt.
The plasmid carries the gene for the immune-prompting protein the vaccine will get your body to make. When the bacteria multiply, researchers get many copies of the plasmid, which they will eventually use to make lots of vaccine.
But this is just the first step for making an mRNA jab — there are six more before you have something that can go into people’s arms (see the sidebar at the end of the article for the full process).

Making an mRNA shot doesn’t need a big production plant. In fact, the development facility at Afrigen spans 380 m2 — about the size of four two-bedroom townhouses next to one another. A setup of this size can produce, theoretically, about three million vials per year, says Caryn Fenner, an executive director at Afrigen. Three million vials will give 30-million doses (because each vial contains enough for 10 shots).
The number of vials that can be pushed out in a certain time, however, depends not only on how long it takes to make the actual drug product (the stuff that goes into the vaccine that makes it work) but also on how long the quality tests take during the process to ensure the jab is safe to use. Fenner says making the drug product can be done in as little as seven days, while the various quality tests can add up to two months to the process.
A hub with spokes
It’s not Afrigen who will mass produce the shots they develop. For that, the mRNA hub model has something called “spokes”.
Spokes are vaccine manufacturers in low- and middle-income countries who the World Health Organisation has chosen to make the jab that Afrigen creates in large volumes.
Spoke companies won’t simply be getting a pack of instructions and then be left to their own devices. Instead, Afrigen’s scientists will train them, with the spokes coming to the hub to learn how to work with mRNA technology. Afrigen researchers will also do on-site visits at spokes’ premises to help them set up their facilities.
“Tech transfer happens on two feet,” says Terblanche.
One of the rules to become a spoke is that the country where a spoke is based must have a medicine regulator who has reached at least level three maturity according to WHO standards, so that the WHO knows there’s an authority who will vet that the products made by a spoke are safe to use and work the way they should.
A level three rating means that the regulator (in South Africa’s case this is the South African Health Products Regulatory Authority, Sahpra) is stable and has “stringent, well-functioning regulatory systems” that are on par with the standards of international authorities such as the United States Food and Drug Administration. Sahpra was awarded this status in early October and a few other spoke countries, such as India, Ghana and Serbia, have received their status too.
Fenner says: “Some spoke companies have fairly advanced setups already, whereas others are building their facilities from scratch. But there’s no set way to design your space: the plant simply needs to meet cleanroom requirements.”

The spoke that is part of the hub’s South African consortium (so the company that will produce thousands of vials for the clinical trials during which Afrigen’s COVID jab will be tested on thousands of people) is the vaccine manufacturer Biovac in Cape Town.
Biovac already has some experience with mRNA technology, because it signed a deal with Pfizer/BioNTech last year to fill, cap and label vials of their mRNA jab.
So far, there are 15 biotech companies in Africa, Latin America, India and eastern Europe that have been chosen as spokes. By the end of September, six of them had already had their first set of training sessions at the hub, learning how to work with mRNA vaccine technology.
Says Terblanche: “The beautiful component of this model is that you scale out [rather than having to scale Afrigen’s production facilities up].
Who will own the hub’s jabs?
The Medicines Patent Pool, a United Nations-backed organisation that helps to negotiate licences for the generic production of medicines, will help the hub to sort out licensing agreements for the jabs that Afrigen develops. Although the intellectual property of the shots will be held by Afrigen, it will be made available to spokes for free and the MPP will help with “defining and negotiating terms and conditions of eventual agreements”.
So when will we see the COVID jab that the hub has developed in use? The WHO says approval in South Africa could potentially be in 2024 and the spokes in countries who receive the technology should be able to secure approval shortly thereafter.
Charles Gore, the executive director of the MPP concludes: “This [the hub] is about empowerment. We cannot fail. This project has to work.”
How are mRNA jabs made?
1. Grow a tank full of bacteria that carry the gene for the target antigen.
Scientists put a ring of DNA (called a plasmid) into bacterial cells. The plasmid carries the gene for the antigen. The bacteria then multiply and so make many copies of the plasmid.
2. Burst open the bacterial cells.
The cells are separated from the liquid in which it grew by spinning it down in a centrifuge (a machine that spins the tubes around a central shaft very fast). They are then burst to release the plasmids. A series of purification steps follow to yield a substance that will eventually contain only the plasmids.
3. Add some enzymes into the mix.
mRNA can only be made from a straight piece of DNA. But because the target gene sits in a closed ring of DNA, it needs to be snipped out. This is done by adding a particular enzyme into the mix. An enzyme is a molecule that helps cellular reactions along.
Another type of enzyme lets the two strings of DNA, which are twisted around each other, separate. And yet another enzyme then makes an mRNA molecule from one of the single DNA strings. This is called transcription.
4. Gather up the mRNA molecules.
The mRNA molecules are extracted from the solution by passing it through a thin tube filled with a solid material. The properties of this material make the mRNA molecules stick to it, after which the column is rinsed to get a solution that contains pure mRNA. This is now called the drug substance.
5. Wrap the mRNA in small fat bubbles.
Now it’s time for formulation. The drug substance (aka the mRNA molecules) is mixed into a liquid that will cause them to become surrounded by small fat bubbles, called lipid nanoparticles. A few other ingredients, such as sugar, salts and other fats, are also added to this mix to make up a concentrated form of the drug product — the stuff that goes into the shot to kick your immune system into gear to make antibodies.
6. Get ready to fill the vials.
Only a very small amount of mRNA molecules is needed in a single jab. So the concentrated drug product has to be diluted (a lot) before it can be put into vials. The diluted form is called the final drug product.
7. Fill and cap the vials.
In the case of Afrigen’s COVID vaccine, each vial contains enough vaccine for 10 doses. Vials move along a small conveyor system and each one gets filled by a machine. Each one is sealed with an aluminium cap and then labelled.
About 30 different quality tests are performed during the production process to prove to a medicines regulator (such as the South African Health Products Regulatory Authority, Sahpra) that the vaccine makes the grade. For example, the developer has to be able to show how well the vaccine keeps over time at different temperatures and humidity levels, what the concentration of the mRNA in the drug substance is and how much mRNA there is in each lipid nanoparticle.
Bhekisisa’s visit to Afrigen Biology and Biovac was funded by the Open Society Foundations.
This story was produced by the Bhekisisa Centre for Health Journalism. Sign up for the newsletter.












