- The Umthombo Youth Development Foundation provides bursaries and mentorship to health science students from poor, rural backgrounds. Despite humble beginnings, these students are achieving exceptionally high pass rates. Here’s why.
- Despite growing up under difficult conditions, Umthombo students are achieving high pass rates in their courses at the country’s public universities.
- Students say apart from financial assistance, the mentoring they get is driving their academic success.
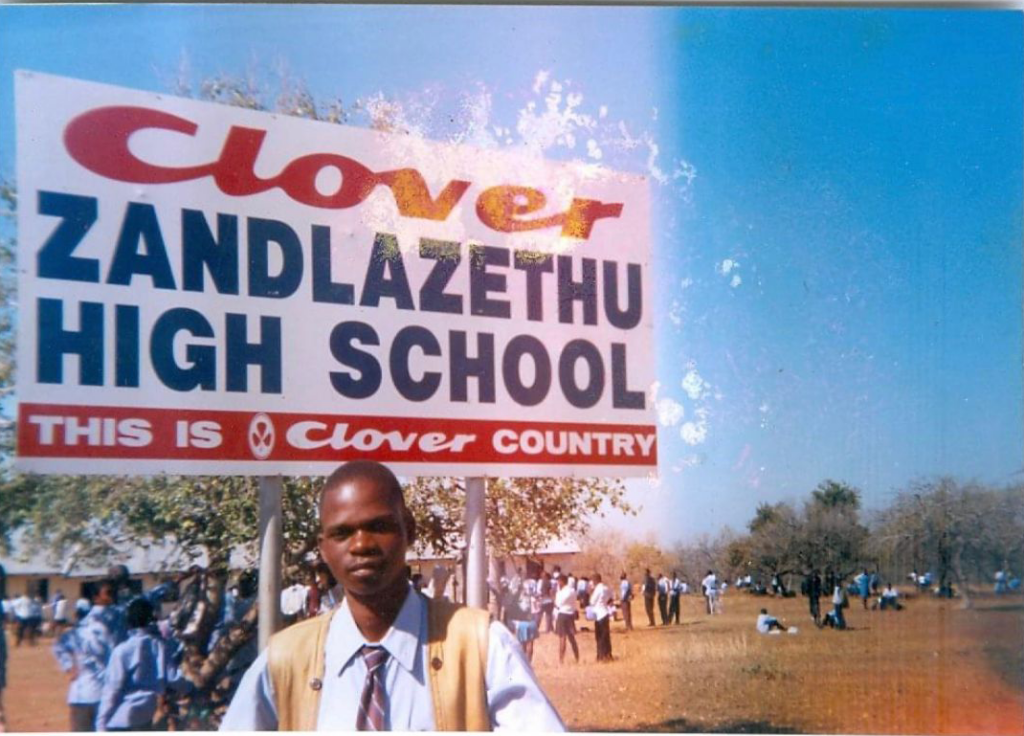
Even by the standards of the poor, rural community in KwaZulu-Natal where Thulani Ngwenya grew up, he had it tough.
There were three categories of people at the high school he attended. One group was driven to school because their parents could afford to pay teachers who had cars. The next bunch could afford a bicycle.
Then there were those who had to walk. “I was in that group,” Ngwenya says.
He would wake up at 4.30am and quickly don his uniform so that he could set off for school by 5am — a journey that could take up to three hours. During winter, most of his walk would be in the dark.
Day in and day out, Ngwenya trudged to school — and back — on an empty stomach. “The meal I had after getting back home was my only one of the day,” he says, smiling from behind a large wooden desk in his office at Bethesda Hospital in Ubombo, a small rural town about 350km northeast of Durban.
Although the facility is just 82 kilometres from where he grew up, Ngwenya has come a long way.
He had to work for a year after matriculating, first as a concrete mixer and then as an informal teacher’s assistant, to earn enough money just to apply to university.
Now, the name tag clipped onto the doctor’s light blue shirt reads “TC Ngwenya, medical manager”.
Poor, rural students excelling in difficult degrees
Ngwenya’s story is remarkable, but it’s not altogether unique.
He’s one of over 500 health workers who come from poor, rural backgrounds and whose studies were supported by the Umthombo Youth Development Foundation. This nonprofit organisation, set up to help fix the shortage of health workers in rural areas, helps keen students to study in the health sciences at South African universities and supports them financially throughout their studies.
A 2011 health department analysis found that less than 3% of South Africa’s medical students end up working in rural areas 10 to 20 years after graduating and that this contributes to a huge gap in people’s access to healthcare between rural and urban areas.
But according to one study conducted at the University of the Witwatersrand (Wits), doctors who come from a rural area are almost five times more likely to work in such places than their peers who grew up in a city five years after graduating. Other research has found similar results.
That’s why Umthombo helps rural students specifically.
Since its establishment in 1999, Umthombo has helped 524 students graduate in health science fields such as medicine, nursing, physiotherapy, speech and language therapy, audiology, occupational therapy and pharmacology.
Umthombo’s grantees get university funding, mentorship and holiday work experience at a state hospital.
The support comes on the condition that graduates return to work in the rural areas in which they grew up for at least as long as Umthombo assisted them during their studies.
To get into the Umthombo programme, prospective students must have been accepted into a health science degree at a public university. They must also be from the rural area around Zithulele Hospital in the Eastern Cape or the rural districts Umkhanyakude, Zululand or King Cetshwayo in KwaZulu-Natal.
Moreover, candidates must have matriculated from a quintile one or two school (these are the poorest 40% of schools in the country, which pupils attend for free).
Umthombo students have achieved great academic success, despite their impoverished backgrounds.
Over the past decade, the average pass rate of Umthombo grantees — the proportion of students who progress to the next year of study — has been 92%.
[WATCH] What makes a good doctor? Why school marks aren’t everything
When Umthombo health science students’ pass rates are compared to those of one of SA’s top universities, Wits, it’s more than 30 percentage points higher: just 60% of undergraduate health science students at Wits progressed to the next year of their studies in 2021.
Health science students at Wits come from different backgrounds, including many from well-resourced public and private schools, but all Umthombo-funded students are from underdeveloped rural communities and attended the country’s poorest schools.
Gavin MacGregor, Umthombo’s director, says that overall, the programme’s support is modest, showing that it’s easy and relatively cheap to help people from poor, rural backgrounds to get good university marks.
MacGregor says the Foundation spends about R56 000 per student each year, though this includes fixed costs like renting offices for programme staff. The average cost of mentoring students is only R14 000 per student per year.
The programme is funded by donors including corporations such as Discovery and Bidvest as well as private individuals such as some of the Foundation’s graduates.
Umthombo’s annual budget was R16.7-million in 2018.
But how does the project work? We travelled to KwaZulu-Natal to find out.

A small nudge goes a long way
Zandile Blose is sitting in an empty classroom on the sprawling Westville campus of the University of KwaZulu-Natal (UKZN), where she’s a lecturer in the audiology department. She’s been a mentor for Umthombo’s students since 2012.
“I meet with the students at least once a month,” she says.
Some of Umthombo’s mentors work at academic institutions where students are based. In other cases, the Foundation’s management meets its mentors at conferences or through university staff.
Mentors are paid R450 per month for every student that they meet with. Some have as little as three students, while others oversee up to 43.
When they’re first hired, mentors are given a template for how they should conduct their monthly meetings and they are required to have in-person meetings with students.
The mentors aren’t necessarily all health workers (although Blose happens to be one), so during training they’re told that their role isn’t to help the students with specific course assignments. Instead they’re tasked with assisting them adjust to university life, to set academic goals and to reflect on how to meet these.
Some of the mentors have been around for more than 10 years, and most stay on for at least five, says MacGregor.
Blose says she tries to be a confidante for her mentees, since many of them have had traumatic childhoods: “I try to develop an open relationship with students so that they can talk to me about their problems.”
To help students keep their studies on track, Blose sits with her mentees at the start of each semester to plan what kind of marks they want to achieve for their different modules. She schedules a monthly meeting with them on the UKZN campus to see how they’ve fared.
“If they meet their targets, we encourage them and help them reflect on what helped them to do well for that particular assessment,” Blose explains.
If they failed to achieve their goals, mentors help students to think about why that happened and to come up with a plan to improve.
For example, if they identified the problem as poor time management, Blose would help students to set up a timetable or work with them to find a different study method.
If there’s a specific subject that they’re struggling with, she finds another Umthombo student who can help.
Mentors often nudge students to ask a lecturer or a tutor for assistance and then follow up regularly to ensure their mentees have actually reached out.
This extra push can make a big difference, says Blose. For students who grew up in deep rural areas, the fact that they have to adjust to a new social environment and have to do everything in a language that’s not their mother tongue can feel intimidating and deter them from asking for help on their own.
Blose says having a mentor to report back to may not seem like much, but in some cases it’s the first time students have ever had someone interested in their academic development.
Ngwenya agrees: “For most of us coming from the rurals, our parents or the gogo that raises you doesn’t know anything about school. No one is asking you about your performance, there’s no one to account to. Umthombo fills that gap.”
Technology is another aspect of university life with which Umthombo students often need help. Blose says she regularly sets up computer tutorials for her mentees from how to switch a device on to lessons on how to use programmes such as Microsoft Word to write clinical reports.
“A lot of our students have never worked with a laptop,” she says.
MacGregor argues that it’s because support starts early and runs for the full first two years of Umthombo students’ studies that it makes such a big difference.
“Some universities do help students who are struggling, but it comes too late. Students often only ask for help after they’ve already failed their June exams.”
[WATCH] How to get doctors to work outside cities
How Umthombo gives students the peace of mind to focus on their studies
In Ngwenya’s Umthombo days (he studied medicine from 2008 to 2012), the Foundation gave full-cost bursaries to students, like him, who would never have been able to afford university studies otherwise.
But in 2018, the National Student Financial Aids Scheme (NSFAS), a government scheme which pays for undergraduate studies, took over this role.
So these days, Umthombo’s financial contribution is more of a top-up bursary, which provides students with extra money for food and books and a stipend to cover the cost of medical equipment and workwear such as lab coats.
But a little goes a long way.
Sibusiso Nxumalo is a fourth-year medical student at UKZN. He’s been on an Umthombo scholarship since 2020, when he was in his second year.
Unlike many other bursaries, which give people a set amount of money at the end of the month, Umthombo’s financial assistance is set up in a more flexible way.
“At one point I needed a stethoscope in the middle of the month, which I couldn’t afford,” Nxumalo recalls. “Umthombo sorted that out for me immediately.”
Students who rely on NSFAS alone often don’t have such efficient access to funds.
Nxumalo says he’s seen some of his classmates struggle to get their course material online if the government-backed aid scheme doesn’t release students’ funding in time for the start of the academic year.
Says Nxumalo: “That financial assistance helps you to be at ease so that you can focus on your studies.”
A holiday job with a big pay-off
One of the first things Umthombo scholarship recipients told Bhekisisa when we asked them about the value of the programme, was that they are required to do holiday work at the local hospital where they first registered for the Foundation’s assistance.
MacGregor says this part of the programme was designed to help students build a connection with the staff at the facility that they will be assigned to work at once they’ve graduated, so that they’re more likely to return once they qualify.
The holiday internships also allow the health workers-in-training to get practical experience early.
Hlobiesile Nkosie, a fourth-year medical student with Umthombo, says: “Having to work in hospitals from our first year onward helps to build experience. By the time you start clinical work at medical school in the third or fourth year, it’s already a lot easier.”
‘I’ve always wanted to stay’
But do Umthombo students stick to their agreements to return to work in the rural areas where they grew up?
According to the nonprofit’s data, which Bhekisisa has seen, Umthombo supported 500 students between 1999 and 2016. Of that number, 415 (or 83%) ended up graduating on Umthombo bursaries.
Almost all of Umthombo’s graduates completed their contractual obligations to work at their local rural hospitals for as long as Umthombo funded their studies, a 2015 study published in the African Journal of Primary Health Care & Family Medicine shows.
From 1999 to 2013, only nine students had bought themselves out of their scholarship, while one student failed to meet their commitment or pay the Foundation back.
Of those who had completed their obligations, 72% continued to work in rural areas thereafter.
But recent budget restrictions at the KwaZulu-Natal health department have complicated matters; the department can no longer guarantee that there would be positions available to Umthombo graduates in the facility nearest to their hometown.
Salaries are one of the biggest costs to the department, so that’s where they started cutting, MacGregor explains. “Hospitals have been under pressure not to employ new people, including our graduates.”
In cases where graduates can’t find jobs near their hometowns, Umthombo helps them to find employment in other nearby rural areas.
Because provincial health departments’ budgets have increased at a slower rate than the intake of medical students, government hospitals “have not always been able to absorb the new doctors produced in the past years [after completing their internships and community service]”, says Nicholas Crisp, the deputy director general in the national health department tasked with implementing the country’s National Health Insurance (NHI) scheme.
The NHI will be like a large, state-funded medical aid, which will buy the same healthcare for everyone, regardless of their income.
“We simply just don’t have the money to fill all vacant positions or to create additional ones,” says Crisp.
In January, the KwaZulu-Natal health department, for example, issued a moratorium on the filling of posts (except for medical intern and community service positions, and those funded by special grants) “until further notice” — despite 29% of doctor jobs at clinics and 9% in hospitals being unfilled at the time.
The moratorium was lifted at the end of March, but solving the shortage of health professionals in the public health sector, and distributing health workers more equally among rural and urban areas, remains one of the NHI’s toughest tasks.
Back at Bethesda Hospital, Thulani Ngwenya says he’s fortunate to be able to treat people in the district where he grew up. He’s also the acting chief executive officer of the facility.
He has no plans to move out of rural KwaZulu-Natal anytime soon, he says.
Many doctors only stay at rural facilities until they’ve completed their training, but Ngwenya wants his community to benefit from his skills now that he has more experience.
He pauses then says: “I’ve always wanted to stay here. I think I’m going to.”
Jesse Copelyn was a health journalist at Bhekisisa between 2022 and 2023.








