Disease-spreading mozzies may be getting wise to our best defences, but science is fighting back.
Ruth Uwamahoro clutched her toddler son tight. The strength of the small boy’s fever burned against the skin of her arms.
It was a cool July morning atop the rolling hills of Rwanda’s Rwamagana district, not far from the capital, Kigali. People were doing their daily chores in Uwamahoro’s village of Gihuke.
But inside her home, Uwamahoro was in a panic.
Less than a year ago, the boy had fallen ill with a high fever and had nearly died.
That time, it turned out to be typhoid. Caused by bacteria, typhoid is most often spread through contact with contaminated food or water, according to the United States-based research organisation, the Mayo Clinic. If left untreated, the disease can be life-threatening.
What if it was typhoid again, she thought, and what if her baby was next?
Uwamahoro hurried her toddler to the local health centre. There, a healthcare worker took one of the little boy’s fingers in hand, swiped an alcohol swab across it and pricked the tiny digit with a lancet. Then she added dabs of the child’s blood into an array of test kits.
Less than an hour later, Uwamahoro received the results.
What she learned scared her even more.
Could a familiar foe be mounting its own defence?
For centuries, typhoid has been a trickster. So closely do its symptoms mimic those of malaria that for much of the first half of the 20th century, there was a whole field of study devoted to what was then called “typhomalarial fever”.
The term has since fallen away and today, rapid tests for typhoid that can be done at clinics have improved health workers’ ability to diagnose it, although they’re still far from perfect, a 2019 article in the British Medical Journal points out.
This test was clear: The boy didn’t have typhoid. But the results brought Uwamahoro little comfort.
Her son, the clinic staff said, had malaria.
More than a decade ago, malaria — a disease caused by certain parasites and transmitted to humans via mosquitoes — was the leading cause of sickness and death in Rwanda. In 2005, hospitals across the country reported 80 000 severe cases, according to that year’s demographic and health survey. Almost four out of every 10 deaths were among children just like Uwamahoro’s who had not yet turned 5.
By 2011, however, the country had cut the rate of new cases by 86% and deaths from malaria at the country’s health facilities had fallen by almost two-thirds, according to the 2014/2015 version of the report. But the World Health Organisation’s (WHO) latest global malaria report shows that Rwanda — the country has a population of 12.3-million — still sees 4.2-million cases each year.
Globally, about 400 000 people annually die from the disease. And one of the best lines of defence against malaria for Rwanda — and the world — is beginning to fail. The world has long relied on insecticide-treated bed nets to ward off malarial mosquitoes, but in the past decade, at least six dozen nations have reported rising rates of mosquitoes that have become resistant to these chemicals.
And Rwanda is among them.
A peaceful night’s sleep?
Each night, Uwamahoro drapes a mosquito bed net over the family’s single worn mattress, hoping to keep the sickness-carrying bugs at bay. She carefully looks the mesh material over, checking for holes and gaps. Although Uwamahoro can’t see it, she knows that a layer of pyrethroids, a type of insecticide, provides extra protection by killing the night-feasting insects.
Pyrethroids have historically been the only class of insecticides that the WHO approved for use on bed nets. When sprayed on nets, this type of insecticide isn’t only effective but it’s also safe for humans when used properly, the WHO found in multiple research reviews.
Her nightly inspection done, Uwamahoro, her husband, and their two young sons duck beneath the net’s folds to settle in for the night.
After her oldest child still got malaria despite using the net, Uwamahoro vowed to be even more vigilant.
So when she spoke to Bhekisisa in September — as the long rainy season began sweeping across Rwanda’s misty mountains, bringing with it a surge in malaria — Uwamahoro declared that she would do whatever she could to protect her family from mosquitoes.
“Malaria can kill children,” she explains. “I have to protect my kids.”
But her son’s malaria didn’t come from a lack of preparedness. The failure likely came from the very bed net she so carefully sets up every night.
Uwamahoro got her net about three years ago, on her first prenatal visit to the clinic after she became pregnant with her oldest. Since then, she’s been careful to keep it hole-free but also clean — washing it when it gets too dirty. She believes the insecticide permeating the fabric is resistant to washing.
But with every wash, her bed net becomes less and less effective.
A different kind of soap opera
When new medicines or medical products come on the market, manufacturers must get approval from national authorities to sell them in-country. But many nations lack the resources to review mounds of data on everything from how safe a product is to how it’s produced. To help bridge this gap, the WHO approves certain products, including bed nets.
Once the WHO greenlights a drug — or, in this case, a type of insecticide-treated bed net — countries know it’s safe to use at home, and big international donors such as the Global Fund to Fight Aids, TB and Malaria can buy it for the countries they support. To get WHO approval, treated bed nets must pass a gauntlet of checks — including how well they withstand washing.
But those washings are done in a lab, at specific intervals and with specific soap. With a machine.
So in 2010, Kenyan scientists put four WHO-approved brands of nets treated with pyrethroids to the test, replicating how regular people like Uwamahoro would actually wash a net: By hand and with the popular washing powder, Omo.
Scientists found that after just 15 washings like this, anywhere between 98% to just less than half of mosquitoes who were able to bite through the nets still survived. The research, published in Malaria Journal, also explained that how well each net held up to the suds depended largely on the brand of net.
Although washing strips insecticides from the surface of treated nets, their fibres do release more of the chemicals. But they have to be allowed to sit for a length of time — what scientists call the regeneration period — to make this happen.
In the 2010 study, Kenyan scientists said they likely did not wait long enough between washings for regeneration to occur — but that reflects what normally happens in real life.
“In a… situations where people live and cook in single-roomed houses,” they write, “nets accumulate dirt from soot and over-handling in a short time, which often results in an increase in washing frequency”.
Worse yet, there’s growing evidence that malaria-carrying mosquitoes are adapting in order to outsmart the conventional group of pesticides used to treat nets. When Rwandan health officials surveyed 45 sites for mosquitoes resistant to pyrethroids, 30 areas had resistance, shows the WHO’s latest data.
“Most people understand that if you take antibiotics, and it’s always the same kind of antibiotics, eventually those bacteria — the bugs that make us sick — develop resistance to those antibiotics. And then you have to switch to different ones,” says Dave Malone, former technical manager with the Innovative Vector Control Consortium (IVCC). The non-profit organisation works to curb diseases like malaria transmitted via insects.
In a 2017 online video, Malone concludes: “The same thing happens with insects.”
Game changer: WHO approves first new class of insecticide to treat nets in 30 years
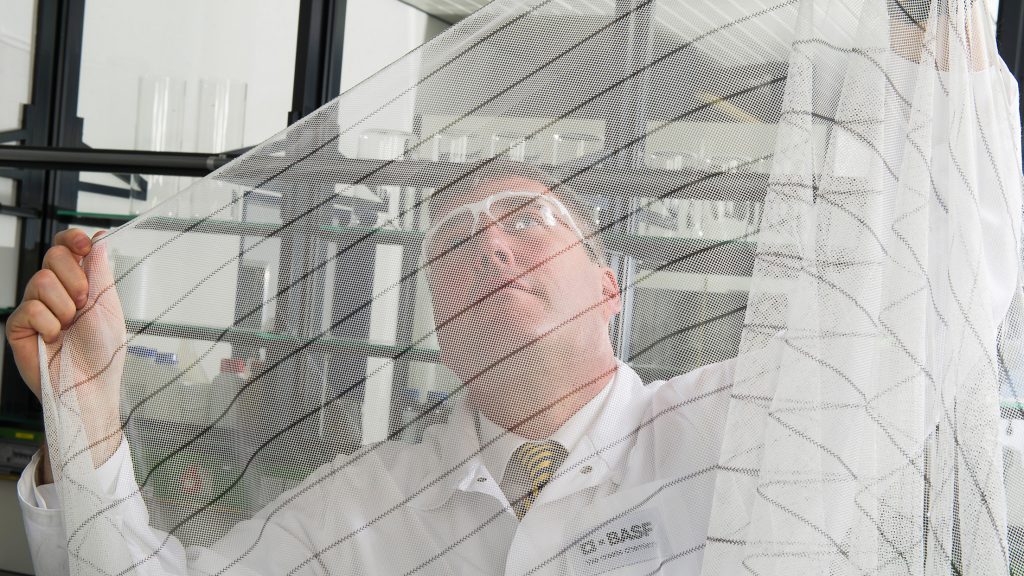
Thousands of kilometres away, James Austin is perched on a chair in front of a long laboratory bench at the offices of global chemical producer BASF. Behind him, under the glow of desk lamps, sit an array of plastic containers.
Resistance, Austin explains in a video for the company, develops when mosquitoes are exposed not only to the same type of insecticides but also to insecticides that are closely related in the way they work.
Imagine: You use the same chemicals to ward off mozzies in an area year after year. In every group, there might be one or five mozzies that hold up a little better against the insecticides. They survive and have babies with, for instance, similar genes that also withstand the next spray. Eventually, these super survivors that are resistant to the chemicals are the only ones left.
Until you change up the game plan.
In 2017, BASF announced it had received WHO approval for an entirely new kind of insecticide-treated bed net, which it dubbed the Interceptor G2. The nets are lined with a mixture of pyrethroids and chlorfenapyr — the first new insecticide combination approved by the WHO to treat bed nets in 30 years, the company says.
The nets were the product of long years of research by BASF in collaboration with the IVCC and the London School of Hygiene & Tropical Medicine that repurposed chlorfenapyr — once intended for use on farms and in homes to battle cockroaches or bed bugs — to help ward off malaria-carrying mozzies.
Chlorfenapyr works by affecting the metabolism of mosquitoes; essentially, it keeps their bodies from producing energy, which is eventually fatal. But it’s a slow death, and that’s why the new nets keep pyrethroids in the mix, says IVCC New Nets Project programme director David McGuire. The idea is that the old staple insecticide will still knock the bugs out, giving the chlorfenapyr more time to course through the insects’ systems.
“When the pyrethroids were working well, they would knock the mosquito down immediately. They’d land on the net, they’d get a little insecticide on them and it would just knock them out and they’d fall to the ground,” he explains. “And they died fairly quickly”.
In 2019, Rwanda began distributing 1.2-million of these next-generation mosquito nets, It’s part of an international pilot programme there and in countries such as Mozambique, Mali and Cote d’Ivoire.
A 2018 trial in Cote d’Ivoire pitted Interceptor G2 nets against, among others, its pyrethroids-only predecessor. It found that even when the Interceptor G2 had been washed 20 times, it still killed 82% of the mozzies that came into contact with it. In contrast, research published in the journal Parasite found that an earlier version of the net, simply called Interceptor, killed only one in 10 bugs after 20 washings — even when washings were spaced out enough to allow nets’ fabric to release more chemicals.
New nets could pack a one-two punch
Today, the transition to new nets, McGuire tells Bhekisisa, is “happening faster than anyone thought because everyone’s realising that the resistance issue with the standard nets is very serious”.
Currently, the Interceptor G2 nets, which come at a higher price, are only recommended for countries such as Rwanda that are encountering resistance to traditional pyrethroid bed net treatments.
Yet many countries across the continent have already confirmed such resistance. According to the WHO, 68 countries already have resistance to at least one form of insecticide, and many other sub-Saharan nations are at risk of seeing resistance develop.
Rwanda is handing out Interceptor G2 nets as part of its regular bed net distribution campaigns, which happen every two to three years. But alongside the novel nets, the government also distributed three-million standard pyrethroid nets and one-million other nets that combine this older insecticide with an added chemical, piperonyl butoxide (PBO), that makes mozzies more susceptible to the pyrethroid.
By making this mix of different types of nets available, researchers will be able to compare how well they perform against one another.
A 2018 research review by the Cochrane centre found that dosing nets with the PBO and pyrethroid combination worked to kill more mosquitoes and prevent more bites than standard pyrethroid-only nets. But the data were not available to determine how long PBO stayed on nets — especially after some research showed it didn’t pass the critical “20 wash” test.

And getting that evidence can take years. BASF, for instance, worked on its G2 net for nearly two decades.
But if the current pilot goes well, it could change the way new insecticide-treated nets are rolled out in the future.
The process for WHO approval on new insecticides for bed nets is long and expensive.
“Before WHO will make a policy recommendation, they require multiple randomized controlled trials over a couple of years in different settings, which is very time-consuming and very costly,” IVCC’s McGuire explained.
It’s important to prove that any new nets are more effective at killing mosquitoes and preventing malaria, he added. But once that’s proven, it doesn’t need to be re-proven, McGuire said.
Future new net projects might only do mosquito-fatality tests, which are much easier and cheaper to conduct.
Back in Gihuke village, Uwamahoro took the malaria medicine offered by the health centre and carefully meted it out to her son, who soon recovered.
Now, he plays on the family’s mattress with other children from the neighborhood laughing and shouting.
Their old bed net is stashed away in the corner. They’ll keep using it every night until they find a new one.
This reporting was supported by an International Women’s Media Foundation fellowship.
[29 February 2020 10:56am. This story was updated to reflect that since the 2017 interview cited, Dave Malone has left the IVCC.]





