- The African Medicines Agency (Ama) — a medicines regulator in the making for Africa — has received over 30 applications from pharmaceutical companies for medicines to approve during its pilot phase, which will last for about a year.
- Ama will be based in Rwanda and will review new medicines and production facilities on behalf of African countries. South Africa’s medicines regulator is coordinating the applications by offering its digital platform for manufacturers to file their documents.
- But South Africa won’t have a say in the appointment of Ama’s board or director general until it ratifies the treaty for the establishment of the agency; 27 African Union member states had ratified it by the end of November.
Mia Malan and Linda Pretorius break down how to get meds to Africa faster in today’s newsletter. Sign up.

The African Medicines Agency (Ama) — a medicines regulator in the making for Africa — has received over 30 applications from pharmaceutical companies for medicines to approve during its pilot phase, which will last for about a year, says Chimwemwe Chamdimba, who heads the African Medicines Regulatory Harmonisation programme and is coordinating the process until a director general for the agency is appointed.
Ama, with its headquarters in Rwanda, will review new medicines and production facilities on behalf of African countries, who can then decide to register the products locally if they want to, without having to go through the costly process of reviewing the data themselves, or, in cases where a country doesn’t have a regulator, wait for World Health Organisation (WHO) approval of a medicine.
Ama’s review will focus on medications for conditions that are public health worries in Africa, such as heart disease and diabetes, or tropical diseases such as bilharzia and sleeping sickness, which don’t crop up often in other parts of the world anymore but affect many poor people on the continent.
South Africa’s medicines regulator, the South African Health Products Regulatory Authority (Sahpra), is coordinating the application process by offering its digital platform for manufacturers to file their documents, says Sahpra’s CEO, Boitumelo Semete-Makokotlela.
But Chamdimba says South Africa is not yet one of the 27 African Union member states who have ratified the treaty for the establishment of the agency, which means the country doesn’t, at this stage, have a say in the appointment of Ama’s board or director general.
Who has ratified the treaty and what does it mean?
The latest country to have ratified the treaty is Tanzania, whose regulator, just like Sahpra, is one of the continent’s top five. These authorities — the others are Nigeria, Ghana and Egypt — have all obtained the second highest level of “maturity status” from the WHO, which means that they’re autonomous (so, they’re independent entities, rather than being part of health departments), stable and functioning well because they have enough staff and good systems in place.
Some other countries who have also ratified the treaty include Zimbabwe, Uganda, Namibia, Lesotho, Kenya, Ghana, Senegal, Egypt and Rwanda.
Ama will lean heavily on the expertise of the continent’s top regulators, in the sense that it will look to them as offering a kind of template for evaluating safety and efficacy data and how to set up systems for approving a product.
Ama was officially established three years ago, on 5 November 2021, as a specialised agency of the African Union. Chamdimba says the goal is to have a nine-member board appointed by the end of the year, who will then make a recommendation for a director general, to be appointed to handle the agency’s day-to-day management. The “conference of the states parties”, who are the countries who have ratified the treaty, will appoint this position.
South Africa signed the treaty in 2022, which means the country officially declared wanting to align with the agency. The treaty was then tabled before the National Assembly and referred to the National Council of Provinces for approval, which the health department’s director for international relations, Moeketsi Modisenyane, says could happen before the end of December. But, he adds. “I don’t have control over parliamentary processes.”
Getting to ratification will, however, take longer than that, as it involves a process with state law advisors. Ratification means the health minister, as a representative of the government, signs a document that shows the country agrees to be bound by the treaty’s rules.
Once South Africa has ratified the treaty, the agreement is legally binding and the country will have to pay annual membership fees, which, according to the treaty, will be set by the participating countries and based on Ama’s needs. How much each country will, however, contribute, will be calculated on a formula similar to the one the African Union uses for setting membership fees, which is based on the size of a country’s economy. This means rich countries pay more for their membership than poorer countries.
Extra funds will come from the fees drug companies have to pay the agency to process their applications, and from donors.
For the most part, Ama will only review medicines that are made up of what drug scientists call “complex molecules” and medication for diseases that are common in Africa, such as HIV, tuberculosis and malaria, says Chamdimba. Moreover, only countries who have ratified the treaty, and have paid-up memberships, will be able to use Ama’s reviews to register medicines in their countries.
An example of a complex-molecule drug is an mRNA vaccine, such as the one used for COVID, or the 3-in-1 anti-HIV pill that contains dolutegravir, tenofovir and lamivudine.
In this case, the substance that creates the treatment or protective effect in the body is made up of different chemicals that are combined in a clever way so that a patient has to take a smaller dose or fewer pills, and have fewer side effects.
How will Ama work?
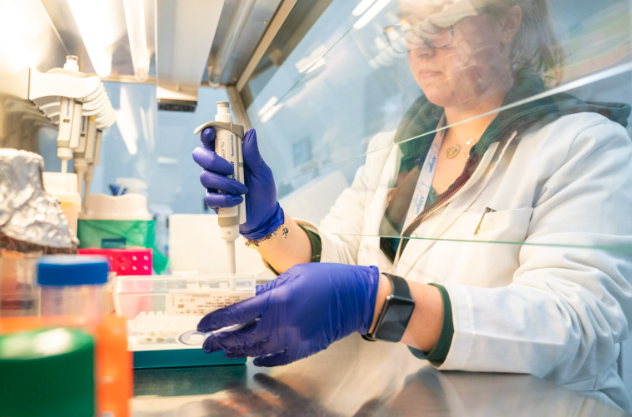
Before a medicine can be put on the shelves, it has to be approved and registered by a country’s medicines regulator. This means that although pharma companies make the drugs, the regulatory body verifies the data that shows how well the drug works and makes the rules about how it can be marketed and sold, so that the medicines we buy are safe and work the way they’re supposed to.
A regulator also has to keep an eye on how people use the medicine, investigate any serious side effects being reported and review data that come from any changes to the medicine.
But this is a long, laborious process — for which many countries in Africa don’t have the expertise, money or laws in place. A regional regulator, with standard quality guidelines, operating methods, documentation and requirements in place, can help to streamline the process for assessing a product and, if it gets the thumbs up, it can be passed on to a country’s local authorities to decide whether they want to register it.
This will mean that people will be able to get new medicines sooner, and not have to rely on products having to get the go-ahead from an organisation such as the WHO — which can take long if you’re at the back of the queue — before it can become available in their country.
If the system for getting medicines registered is thorough and sticks to strict quality checks — and there are Ama officials who keep track of how products are used in the region — it can also mean that the gap for falsified drugs going around can shrink, says Semete-Makokotlela.
However, having a central medicines agency doesn’t necessarily mean that if a product passes their assessment that countries will be obliged to have it in their pharmacies. Instead, member states will still be able to decide whether they want to accept Ama’s recommendation and, if so, what information has to be included in the product pamphlet or the packaging.
For the plan to work, though, members have to hold one another accountable, Semete-Makokotlela adds. “It cannot be that we signed up for these mechanisms and then when it comes to the country, they want to do another level of assessment. It defies the whole process.”
A real-life example
A case in point? Take the South African drug company Kiara Health’s planned manufacturing of the monthly dapivirine vaginal ring, which can lower a woman’s chances of contracting HIV through sex by about 30%. The ring has been registered in 11 African countries, including South Africa. But each of those countries had to review the results from lab tests and clinical trials submitted by the International Partnership for Microbicides, who developed the ring, individually.
If Ama had been running fully when the ring became available in 2021, the countries who have ratified the Ama treaty wouldn’t each have had to review the efficacy data themselves. Instead, they would have been able to use Ama’s review. Moreover, says Kiara Health’s CEO, Skhumbuzo Ngozwana, when Kiara Health starts to make the ring (no date has been set yet), Ama could inspect Kiara Health’s manufacturing facility and make a recommendation, instead of teams of each country having to fly into South Africa to assess the premises.
That way, the company is able to process countries’ orders quicker, because the quality of their product is endorsed fast yet thoroughly.
Ngozwana explains: “A well-functioning regulatory system is the bedrock of any pharmaceutical industry; most importantly, it’s the guardrail that protects public health.”
Same, same: Is Ama and Ema the same thing?
The thinking behind setting up a shared medicines regulator for Africa is similar to that of the European Medicines Agency (Ema), says Chamdimba, in the sense that people and goods can move freely between countries that are part of the Schengen area. This is an area where border control between countries doesn’t apply and covers most countries in the European Union, such as Germany, France, Italy and Croatia.
But Ama won’t be an exact copy of Ema, says Chamdimba, “because we’re learning from what has worked already”. By following the Ema example but adapting it for what countries in Africa need, the agency can get going soon.
“It shouldn’t take 15 years,” she says of the slow-going until now. “It must take less because of having learned from what has happened in the European agency.”