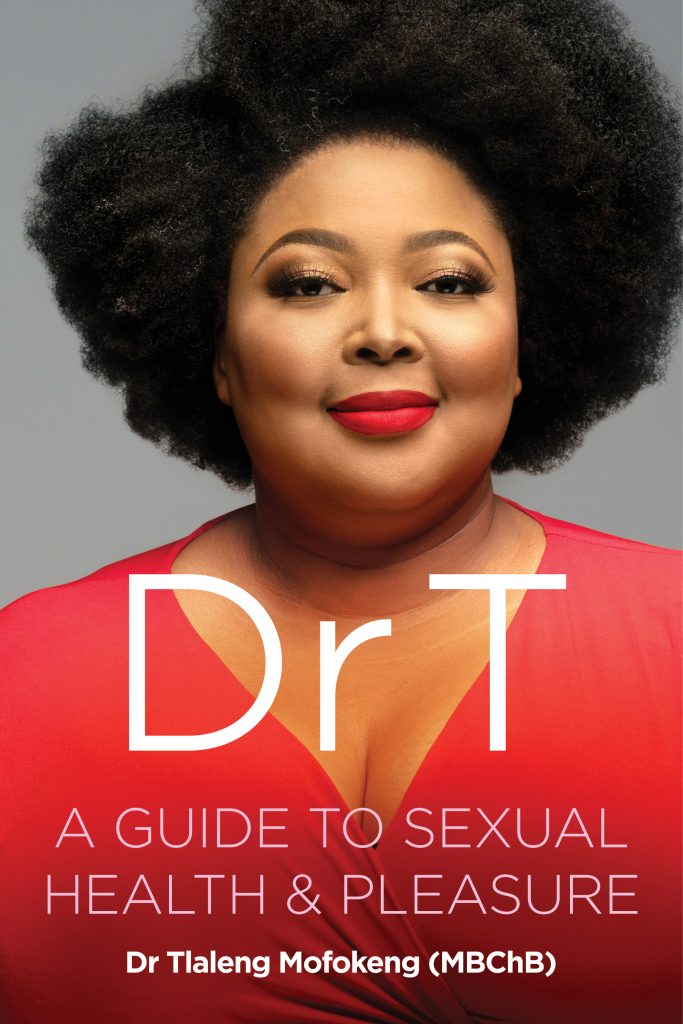
- Tlaleng Mofokeng is a doctor, writer, radio and TV presenter as well as an internationally-renowned health activist. She’s made it her life work to educate people on sexual and reproductive health and rights and her first book is a primer on everything from anal sex to intersectionality.
- Read why medical school never prepared her for becoming ‘the sex doctor’ in this excerpt from her newly released first book, “Dr T: A Guide to Sexual Health and Pleasure.”
COMMENT
As a junior medical student, it became clear that even in medicine women’s pleasure is not prioritised.
One of the most daunting, but also exciting, aspects of the first year of medical school is human cadaver dissection. I don’t know why, but even then I was already inquisitive and aware of how little focus was given to female genitalia, specifically the anatomical teachings of the vulva and clitoris, even in that basic introduction to human anatomy.
During obstetric and gynaecology lectures and tutorials at a senior level, the focus of the content was on sexual illness and disease — and not nearly enough on pleasure.
One would think that, for example, when discussing contraceptive methods with known side effects such as vaginal dryness, negative impact on libido and the desire for sex and mood changes, women’s sexual pleasure and solutions to these issues would be a key area.
But discussions regarding women’s health have been devoid of affirming information surrounding sexual pleasure.
In contrast, what one learns in urology surrounding male sexual dysfunction, biomedical research and solutions around weak erections and early ejaculation, surpassed the equivalent of anything available regarding women’s pleasure, even in curricula.
Those of us who had developed an interest early on about sexual and reproductive health in relation to women’s experiences were let down by our textbooks and additional course work that lacked depth and a variety of research on these topics.
The current time demands us as health professionals to be better.
Unfortunately many healthcare professionals, in their own childhood development, have not received comprehensive sexual education. As a result, they can perpetuate myths, gender and sexuality biases or discrimination in their patient interactions based on unchallenged prejudices.
Providing personal development for young and old medics alike through a sexual reproductive health and rights framework during undergraduate training and as part of postgraduate continued medical education is vital.
Having graduated and being acutely aware of how low sexual pleasure was placed in medicine… I very quickly developed a bias towards women’s health and creating clinical services affirming of women’s needs.
As someone who is a woman and was assigned female at birth, I identify as a cisgender woman. I still felt that my sexuality and sexual health were being under-represented, so what then of transgender women waiting to receive affirming healthcare?
Or young people born with HIV … where the current prevention messaging is altogether missed from their reality? Or women sex workers who require very specific occupational information and screening tests?
And all of us dealing with the various medical conditions I have discussed in the previous section?
I didn’t always know what field of medicine I would specialise in and ultimately end up in, so becoming ‘Dr T the Sex Doctor’ was the most organic and fulfilling experiences of my life.
Meeting women, hearing about their experiences, thoughts, feelings, how we as women experience our bodies through menopause, menstruation and through sexual violence and trauma and what that would look like, not just for women in general but for South African women, became my focus.
It was only once I started doing work on radio, in print and hosting sex toy parties, when I realised a lot of what I knew to be true for myself was affirmed by other women’s experiences.
Tlaleng Mofokeng
South Africa has very specific circumstances in that not only was there previous legislative violence that came with apartheid but also healthcare was not designed for black women. We are also living in a country where the extremely high levels of sexual violence, harassment and rape mean that not only do most of us know someone who has been violated in some way, but many of us carry with us experiences that we are not always sure of in terms of what they actually ‘mean’.
It was only once I started doing work on radio, in print and hosting sex toy parties, when I realised a lot of what I knew to be true for myself was affirmed by other women’s experiences.
Often when you have deep meaningful conversations with patients they tend to become less of the typical doctor/patient conversations, and often you are challenged in ways you aren’t always ready for.
I did not always know or have all the answers so I became a student of my patients. We were both ‘giving and taking’ within the consultations. There was also something very meaningful in not having time constraints when consulting. People valued that I was taking them seriously when they mentioned a sexual health or sexual pleasure-related issue.
My extended reading had started to include menopause, as well as the contraceptive pill and the adverse effects that come with it so I started developing a way of consulting that offered people information without them asking.
If I heard someone was on a contraceptive, I would then offer them information about lubricants, the link to contraception and how they could expect certain side effects with different contraceptives.
What often caught me off guard was how correct my intuition had been as a young medical professional, not being given any of the information and even finding the necessary information was difficult. I knew then that my feelings of inadequacy were valid.
I did not always know or have all the answers so I became a student of my patients. We were both ‘giving and taking’
Tlaleng Mofokeng
Often I would need to refer and read and find information and find other doctors and writers who had different ways of practising medicine and reproductive health and that has really determined a large part of my career path and the spaces that I currently find myself in.
It has been an experience of growth for me not only as a doctor but personally because I have allowed myself to take and be a part of a journey and immerse myself within the experiences and the stories.
Not only do I open myself up to new experiences from very different people, from all walks of life and of all ages, they feel heard and know I take them seriously.
Many patients I see often have the same history. Whether its how many doctors they’ve consulted and none of them seem to be able to help, or no one takes them seriously regarding vaginal dryness or how someone can be raped and still want to enjoy sexual pleasure, these are recurring themes and issues.
I am walking that road with all my patients who come in for therapy and sexual health-related consultations and feel like they have all chosen me to walk this path with them. And for that, I’m lucky.
Tlaleng Mofokeng’s new book, “Dr T: A Guide to Sexual Health and Pleasure”, is published by Pan MacMillan. Follow her on Twitter @drtlaleng. This extract was originally published on 5 August 2019.
Dr Tlaleng Mofokeng is a United Nations special rapporteur on the right to health and the author of Dr T: A Guide to Sexual Health and Pleasure. She's the former vice-chairperson of the Sexual and Reproductive Justice Coalition and also a former member of the Commission for Gender Equality in South Africa.




![[WATCH] Busted: Three myths about drug addiction](https://bhekisisa.org/wp-content/uploads/2023/06/c1bb5976-00-bluetooth-the-myth-that-fooled-a-nation-150x150.jpeg)

