- Despite progress in tackling tuberculosis (TB) in the five years since the last high-level meeting at the United Nations General Assembly in 2018, none of the targets set out then have been met. Governments have, for instance, not spent close to the amount of money they said they’d spend on TB.
- Today, political leaders will be talking about how to get back on track to end the disease by 2030 — but can they be trusted to stick to their commitments?
- Expensive medicines and patents which are extended beyond the initial 20 years are some of the issues that are blocking faster progress.
- We’ve spoken to three people about their journeys with TB — and why it’s important to hold political leaders accountable for commitments they make at meetings like today’s.
In 2018, at the last high-level meeting on the fight against tuberculosis (TB) world leaders adopted aspirational goals to get us to ending TB by 2030.
Five years later, the talks at the United Nations General Assembly are on again — in the shadow of much of the progress in reducing the burden of TB since then having been reversed because of the COVID-19 pandemic.
Despite at least some progress in tackling TB over this period, none of the targets set out in 2018 have been met — something the delegates at today’s discussion say is “deeply concerning” in a draft declaration.
In 2021, about 10.6-million people got sick with TB and 1.6-million died. But TB is a preventable and curable disease — if it’s caught early. Worryingly, the number of cases of multidrug-resistant TB (MDR-TB) rose by 3.1% in 2021, which the declaration says poses “a critical challenge that could reverse the progress made against the disease”.
MDR/RR-TB, a type of TB for which standard treatment doesn’t work, often develops because people get onto treatment too late — be it because of unfair pricing or struggling to get tested.
In an unprecedented move, South Africa’s Competition Commission announced last week that it will investigate the American drugmaker Johnson & Johnson (J&J) for the high price it has been charging the country for bedaquiline, as well as for extending the tablets’ 20-year patent until 2027 to block cheaper generics from entering the country.
Bedaquiline is used to treat MDR-TB and is mostly used in combination with other medicines. It has to be taken for six months and is considered a game changer because it has replaced treatment — up to two years of long, painful injections with serious side effects (such as hearing loss) — with lower cure and higher death rates.
We’ve put together three people’s stories on how TB — and the struggle for access to medicines — has affected their lives. It’s accounts like these that underscore the importance of of leaders being held accountable for following through on commitments made at high-level discussions such as today’s.
I survived the most deadly type of TB, but it cost me a lung

“One day in 2012 I started coughing up blood. It was a Monday.
“My doctor sent me to a public clinic where they took my sputum [sputum is another word for phlegm — the mucus that people cough up from the lungs]. I went back on the Friday and they told me I had multidrug-resistant tuberculosis. It meant that the usual TB treatment available then [a course of antibiotics for about six months] wouldn’t have worked for me.
“The doctors and nurses assumed I had had TB before and had stopped taking my medication, and that’s why I got this form of the disease. They blamed me for it.
“But I have never been on TB medicine before. I had contracted a drug-resistant bug from the start.
“About three days later, I went back to the clinic to start my treatment.
“When I saw the doctor, he had to go look at a flip chart behind the door [to see how to treat me].
“I was shocked that the chart seemed hidden away. It showed me that the health workers in that clinic didn’t really care to know more about the condition.
“It was as if they expected people with MDR-TB to die.
“I had to get an injection of kanamycin [an antibiotic] every day for nearly six months [along with four other drugs, which had to be taken for 18 more months].
“Towards the end of my treatment, the drugs stopped working. The doctors told me I now had extensively drug-resistant TB [also known as XDR-TB], a very serious variant of the disease that wouldn’t respond to even the most powerful TB medication clinics had at the time.
“They had no idea why this happened. For months I had responded well to the treatment, they said.
“The only option was to take a drug called linezolid. But it wasn’t widely available in the country at the time and you had to wait for about a month to get it.
“By the time I got my first dose of this medicine, the TB bacteria had already destroyed my one lung.
“Fearing that the disease would spread [to other parts of my body], the doctors removed my damaged lung.
[WATCH] How to use pills to prevent TB
“I was put on a new course of medicines, which included bedaquiline, delamanid and linezolid. Eventually, after four years of TB treatment, I was cured.
“I nearly collapsed when my doctor phoned me with the news, because I had started thinking that I’ll have to take up to 40 tablets every day — like I had done for most of my treatment period — for the rest of my life.
“I’m afraid of contracting the disease again. I would rather die than to go back on all that medication [even though treatment for MDR-TB is only nine months today].
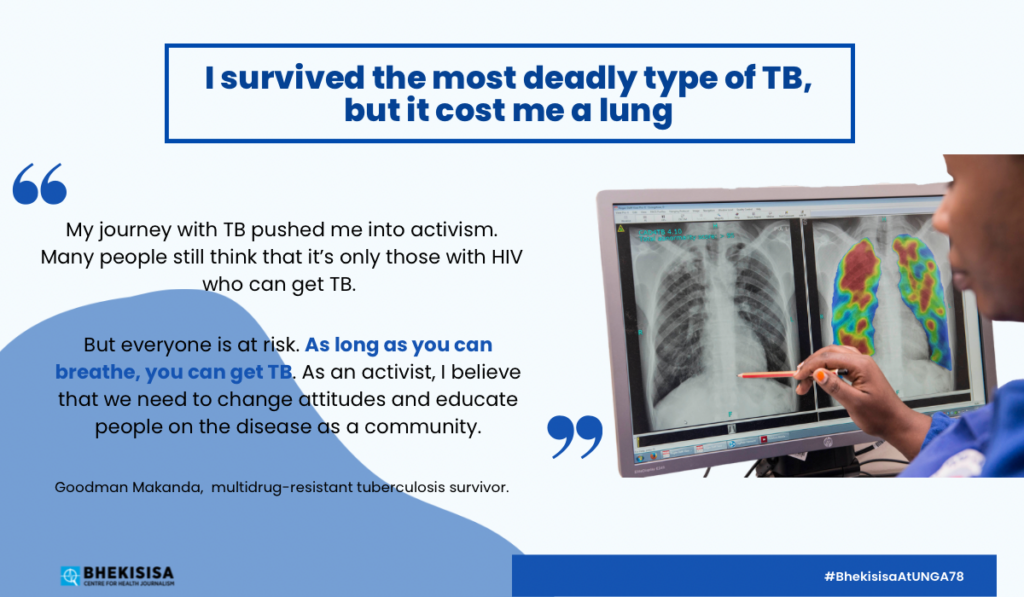
“My journey with TB pushed me into activism. Many people still think that it’s only those with HIV who can get TB.
“But everyone is at risk. As long as you can breathe, you can get TB. As an activist, I believe that we need to change attitudes and educate people on the disease as a community.”
Although TB is curable, its consequences linger long after treatment for 20–30% of TB survivors; in poorer countries the number might be even higher. The tentacles of the disease reach beyond just the airways, though — scientists are researching how post-TB lung disease affects other body parts (like joints, muscles and the spine), mental health and patients’ quality of life.
I took on Big Pharma and won
“I remember getting sick in 2010, around the time of the Soccer World Cup.
“I was a university student at the time. I did not have symptoms like coughing and sweating [which are typical signs of TB], but I was losing weight dramatically.
“At the campus clinic, the nurse could not find what was wrong with me, so she told me to go see a private doctor.
“The doctor could not find what was wrong with me either. He suggested I get tested for TB.
“The test results came back after three weeks. They were negative.
“I was eventually diagnosed with TB after the doctors did an X-ray of my chest. They found holes in my lungs. I started treatment [with a series of antibiotics] immediately.
“The medicines made no difference.
“The doctors tested me a second time and found that I had MDR-TB. They explained what it is [a type of TB for which the normal antibiotics don’t work]. I didn’t care. I just wanted to get better.
“The nurses told me I couldn’t go home because I could infect other people.
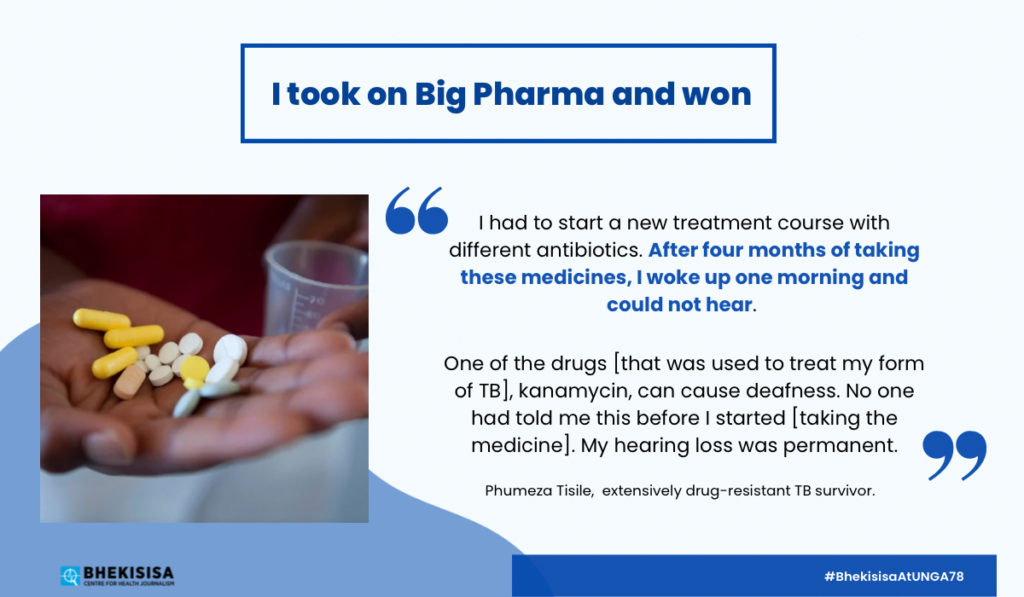
“I had to start a new treatment course with different antibiotics. After four months of taking these medicines, I woke up one morning and could not hear.
[LISTEN] Is this the new TB patient? About half of infected people don’t have symptoms
“One of the drugs [that was used to treat my form of TB], kanamycin, can cause deafness. No one had told me this before I started [taking the medicine]. My hearing loss was permanent.”
Kanamycin is given as an injection deep into a muscle, which is painful. The treatment for MDR-TB has since changed and a drug called bedaquiline is now used. Hearing loss is not linked to taking bedaquiline.
“At the time I lost my hearing, I had developed pre-extensively drug-resistant TB (pre-XDR-TB). [This is a forerunner to a form of TB in which very few of the drugs used to treat the disease will still work.]
“I was moved to [a special] ward. Doctors also found an abscess [a pocket full of pus] on my one lung. They cut it away in an operation, but it left me with broken ribs and a collapsed lung.
“After nine more months of treatment, the medication stopped working again. I now had full-blown XDR-TB. My doctors said I had a 20% chance of surviving.
“But there was [a new] drug they could try, they said. It was a medicine called linezolid.
“I had nothing to lose. I could choose between dying slowly without medication or taking a chance on the new drug.
“Nearly four years after I was first diagnosed with TB, I was cured of XDR-TB.”
Voices from civil society groups are important in the world’s TB fight. For example, in March, the Indian government rejected an application from J&J to extend their patent on bedaquiline. One of the things that helped the officials reach their decision was a petition Phumeza Tisile, who had extremely drug resistant (XDR-TB), filed along with Indian TB activist Nandita Venkatesan in 2019. Without the patent that allows J&J to be the only manufacturer, generic versions of bedaquiline can now be made by other pharmaceutical companies — which means the medication can sell for much cheaper.
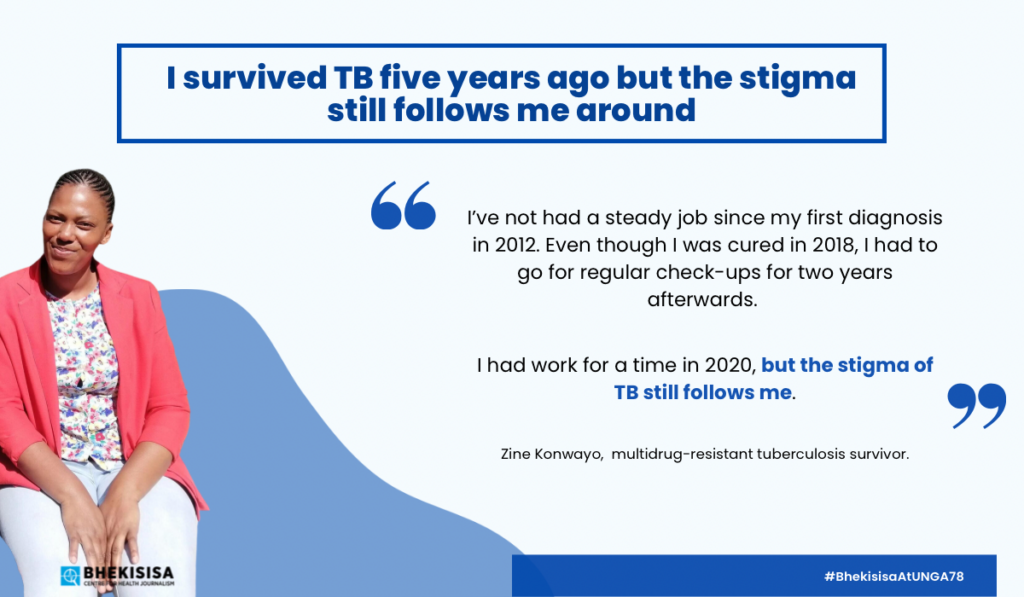
I survived TB five years ago but the stigma still follows me around

“In 2010, my fiancé passed away from tuberculosis (TB). His doctors told me to go to the clinic immediately if I had symptoms like his.
“So in 2012, when I started coughing and losing weight, I got tested. I was diagnosed with MDR-TB, a form of the disease for which one of the normal antibiotics, rifampin, does not work.
“I was admitted to the Fort Grey TB hospital [which has since been closed] for three months.
“When doctors tested me again [after this treatment], they found I had extensively drug-resistant TB (XDR-TB). [This is a form of TB in which very few of the drugs used to treat the disease will still work.] I only started recovering once I was given [a new type of drug called] linezolid.
“In 2015, I tested negative for TB. I was finally discharged.
“That same year, I moved to Cape Town. I felt fresh and healthy. I even gained weight.
“The feeling didn’t last long, though. A few months later, I started coughing up blood while on my lunch break at work.
“I was rushed to hospital, and a chest X-ray showed that I had an abscess [a pocket filled with pus] on my left lung. The abscess had been there for a long time.
“Again I was admitted. This time around I spent two years at Brooklyn Chest Hospital [in Cape Town]. The XDR-TB was back.
“Doctors told me they couldn’t operate on my lungs to remove the abscess [because my body was too weak for surgery]. So they taught me how to do postural drainage [lying or sitting in a series of positions while coughing to get fluid out of the lungs].
“I did this three times a day.
“I was cured of TB in 2018. But my lungs have been damaged and I still struggle to breathe.
“I’ve not had a steady job since my first diagnosis in 2012. Even though I was cured in 2018, I had to go for regular check-ups for two years afterwards.
“I had work for a time in 2020, but the stigma of TB still follows me.
“Employers are hesitant to hire me and they want written confirmation from my doctor that I’ve been cured.
“The state of my lungs also limits where I can work. For example, I can’t work in cold places, because my lungs won’t be able to cope.
“Two years after my last check-up, I’m still looking for work. My age is starting to worry me. I’m turning 36 this year — and the gap in my CV is getting longer.”
A 2022 study in South Africa found that TB makes poor people even poorer. Like Zine Konwayo, people diagnosed with TB often struggle to earn an income because they can no longer do physical work or have to go for lengthy treatment. The cost of being ill with TB equals, on average, 58% of a patient’s individual income, which includes spending money on transport to get to treatment centres and buying food.
But TB rarely affects just the individual. For households caring for a TB patient, the disease amounts to 39% of the home’s collective income. Even though treatment for TB is free in South Africa, buying nutritious food and struggling to get a disability grant make life harder for many TB patients who are already vulnerable.




